Web Portals
Bowel Cancer Symptoms - 'The First two Signs'













Bowel cancer symptoms: The ‘first two' signs of the disease - ‘notice it and follow it up'
Labelled as the "most common cancer" type, bowel cancer targets almost 43,000 people in the UK. The good news is that this diagnosis can be treatable and curable. Doctor Suba M, the director of Science, Health and Wellness at Holland Barrett, has named the "first two" signs of the serious condition.
The bowel describes the part of your digestive system which plays a role in breaking down food and getting rid of waste out of your body.
Due to the location, bowel cancer can present with symptoms that appear when you visit the loo.
And being able to identify these symptoms could help spot the cancer early.
Doctor Suba has outlined the first signs linked to the disease.
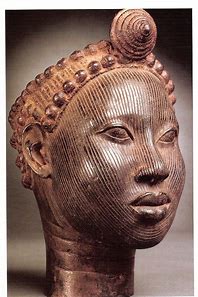
Bowel Image
She said: "Usually, it's kind of blood that's mixed in with the stools that you kind of worry about [and] change in bowel habits.
"These are the first two things that you think about."
Change in bowel habits can include anything from pooing more often to having looser and runnier poos, according to the NHS.
The other common bowel cancer sign - loss of weight - "tends to happen much later", according to the doctor.
According to Doctor Suba, if these symptoms are persisting for more than two weeks, then it might be time to visit the doctor.
She added: "It's not usually just one thing and if you have bowel movements with a bit of blood, don't be alarmed, notice it but then make sure that you follow it up.
"But if you do have any symptoms, definitely get that checked out.
"Not all people who have these symptoms will end up being diagnosed with it [bowel cancer] but it's better to get it checked out."
Change in bowel habits can include anything from pooing more often to having looser and runnier poos.
According to the NHS and Cancer Research UK, other symptoms of bowel cancer include:
- Abdominal pain
- Discomfort or bloating always brought on by eating
- Feeling of needing to empty bowels even after just doing so
- Lump in the back passage
- Tiredness.
The NHS explains that these symptoms need to be taken "more seriously" as you get older or when they persist.
Doctor Suba said: "If you're over a certain age and you're eligible for NHS screening, please, do that, I know it feels a bit uncomfortable ...but I would highly recommend people to do that."
How can I cut my risk of bowel cancer?
The doctor shared: "The main thing is [to eat] fresh whole food and make sure that you're not taking lots of ultra-processed or inflammatory food.
"It's not about one thing because the risk is multifactorial.
"But making sure that you take as much fibre and keep your bowel moving is far more beneficial than any specific superfood.
Doctor Suba has recently helped to give the Bristol Stool Chart a makeover 25 years after its creation to help Britons understand what they are passing and get them talking about their gut health.
Statin intolerance is over-estimated















Statin intolerance is over-estimated
Side effects from statins are overblown and much less common than thought, the largest study of its kind suggests.
Millions take the cholesterol-busting pills every day, in order to cut their risk of heart attack and strokes.
Up to half of patients stop taking the drug, cut their dose or take it irregularly due to suspected side effects, which can include muscle pain, digestive problems and headaches.
Researchers in Poland, however, say as few as 6 per cent of statin users will actually develop 'statin intolerance'.
Professor Maciej Banach, a cardiologist from the Medical University of Lodz, said his team's findings, based on a review of 170 existing studies involving 4million people, show statins 'can be used safely in most patients'.
He said it is 'critically important for reducing their cholesterol levels and preventing heart and blood vessel diseases and death'.
Provided by Daily Mail Statins (pictured) work by limiting the production of 'bad cholesterol' — low-density lipoprotein (LDL) cholesterol — which can harden and narrow the arteries and increase the risk of cardiovascular disease. Previous studies have found that the 'gold-standard' cholesterol-lowering drug will prevent one heart attack or stroke for every 50 people taking it over five years
Statins work by limiting the production of 'bad cholesterol' — low-density lipoprotein (LDL) cholesterol — which can harden and narrow the arteries, and increase the risk of cardiovascular disease.
Studies have repeatedly proven the medicine, which cost less than £5 for a month's supply, saves lives.
Charities claim around 8million Britons and 35million Americans are prescribed the drugs, which should be taken daily.
Doctors believe tens of thousands of people die every year because they shun the life-saving pills, often due to side effects.
The researchers reviewed 176 studies on the rate of statin intolerance, including a total of 4.1million patients.
Participants were aged 60 on average, and 40 per cent were female.
After following the patients for around one-and-a-half years, the researchers found 9.1 per cent of patients showed signs of statin intolerance — when people are forced to stop taking the drug due to its side effects.
But using a different criteria to measure statin intolerance showed the problem was even less common.
Just 6.7 per cent of participants met the threshold in the International Lipid Expert Panel definition — an inability to tolerate a dose of the drug.
A different definition by the National Lipid Association, which considers intolerance to be 'any adverse effects' leading patients to stop the medication, found 7 per cent of people were intolerant.
But the rate stood at just 5.9 per cent under the European Atherosclerosis Society's definition, which defines statin intolerance as people who experienced side effects in their muscles.
Over-65s, women, the obese and black or Asian adults were more likely to suffer side effects, according to the study published in the European Heart Journal.
Taking a higher dose of the drug was also found to increase the risk.
The researchers said it is 'critically important' for medics to know which groups were at risk from statins so other treatments can be considered, such as a lower dosage or other drugs.
Professor Banach said: 'I believe the size of our study, the largest in the world to investigate this question, means we are able to finally and effectively answer the question about the true prevalence of statin intolerance.
'Our findings mean that we should evaluate patients' symptoms very carefully, firstly to see whether symptoms are indeed caused by statins.'
He said doctors should also evaluate whether patients' perceived side effects could be as a result of their 'perceptions that statins are harmful'.
This so-called 'nocebo or drucebo' effect could be responsible for more than 50 per cent of all symptoms, rather than the drug itself, Professor Banach said.
Professor Banach added: 'These results clearly show that patients needn't be afraid of statin therapy as it is very well tolerated in as much as 93 per cent, which is similar or even better than other cardiology drugs, including ones for reducing blood pressure and clotting or blocking of blood vessels.
'What is more, patients need to know that statins may prolong their life, and in cases where side-effects appear, we have enough knowledge to manage these effectively.
'The most important message to patients as a result of this study is that they should keep on taking statins according to the prescribed dose, and discuss any side-effects with their doctor, rather than discontinuing the medication.'
Reference: Emily Craig Health Reporter For Mailonline
Three jabs a year of new drug could save eyesight in 800,000 Brits
Three jabs a year of new drug could save eyesight in 800,000 Brits
Two eye conditions that cause blindness can be treated with a breakthrough drug that dramatically slows the loss of vision.
The medication, faricimab, could soon be offered to people with wet age-related macular degeneration (wet AMD), a leading cause of vision loss in over-60s, and to sufferers of diabetic macular oedema, an eye problem linked to diabetes.
Previous treatments for the conditions had to be given via an injection into the eye once a month, but the new medication is so effective just three jabs a year are needed.
Experts say this could herald a 'significant change' to the way both conditions are treated on the NHS.
Provided by Daily Mail The medication, faricimab, could soon be offered to people with wet age-related macular degeneration (wet AMD), a leading cause of vision loss in over-60s, and to sufferers of diabetic macular oedema, an eye problem linked to diabetes (stock photo)
Faricimab stops fluid leaking into the eye, which is what causes the damage in both wet AMD and diabetic macular oedema.
This is similar to how current treatments work – however, studies suggest faricimab works far better, meaning it can be given less frequently.
A worldwide study revealed that nearly half of faricimab patients were able to go four months before needing another injection, while three-quarters were able to go three months or longer.
Professor Ian Pearce, investigator on the trial and clinical ophthalmologist at Liverpool University Hospitals NHS Foundation Trust, said: 'The option to extend the interval between injections would be really welcomed by patients and would be a significant change.
'With no treatment, these patients could lose their vision in a matter of weeks, but equally no one particularly likes having a needle stuck in their eye.
'This drug has the potential to make a big difference to patients' lives and allow them to spend less time in hospital.'
While wet AMD and diabetic macular oedema are separate conditions they share the same cause.
In both, damage to the blood vessels near the eye leads to swelling in the macula, a patch of light-sensitive cells at the back of the eye responsible for central and fine-detail vision needed for tasks such as reading.
With wet AMD, which affects more than 600,000 Britons, abnormal and fragile blood vessels begin to grow under the macula for reasons not fully understood.
These begin to leak blood and fluid, putting pressure on the macula. Sufferers will usually first notice the middle part of their vision is blurred or distorted. Left untreated, this can lead to near-total loss of vision within weeks or months.
For those with diabetic macular oedema, the speed of degeneration is slower.
Over time, high blood sugar caused by diabetes can damage the tiny blood vessels near the eye, and fluid can begin to seep out and build up around the macula.
While it can take several years before diabetic macular oedema leads to severe sight loss, because it develops earlier in life than AMD it can have a profound effect on the more than 200,000 UK sufferers.
'It doesn't take much vision loss to impact your ability to carry out day-to-day activities like driving,' said Prof Pearce.
While some patients can receive light or laser therapy to destroy faulty blood vessels, the majority of people will receive injections directly into the eyeball.
These jabs target a protein in the blood called VEGF which can cause abnormal blood vessels to form.
Developed by pharmaceutical firm Roche, faricimab blocks production of VEGF in a similar way but is the first medicine to also reduce the level of a compound in the blood called Ang2, which at high concentrations can lead to leakage in blood vessels.'
Philip Rumsby, 40, from Liverpool, was one of the first Britons to receive faricimab after he developed diabetic macular oedema four years ago.
The call-centre analyst had been living with type 2 diabetes for ten years before the condition developed.
'I noticed something was off with my right eye. It was blurry and my vision had got worse in general, especially when reading. Being diabetic, I get regular eye check-ups, so within a few months the doctors picked it up.'
Philip was started on the faricimab trial and, at first, the injections were given every month. But after two years this was extended to every 12 weeks.
'It really works,' said Philip. 'I don't get the blurring any more and my vision's improved too. The doctors showed me a scan. At the beginning there was loads of fluid in my eye. Now it's all gone.'
Doctors have told Philip that the time between his injections could soon be extended again. He added: 'If the drug keeps working as it is now, they might extend it by another month or even more.'
Reference: Ethan Ennals For The Mail On Sunday
Articles - Most Read
- Home
- LIVER DIS-EASE AND GALL BLADDER DIS-EASE
- Contacts
- African Wholistics - Medicines, Machines and Ignorance
- African Wholistics -The Overlooked Revolution
- African Holistics - Seduced by Ignorance and Research
- The Children of the Sun-3
- Kidney Stones-African Holistic Health
- The Serpent and the RainBow-The Jaguar - 2
- PART ONE: DIS-EASE TREATMENT AND HEALTH-3
- 'Tortured' and shackled pupils freed from Nigerian Islamic school
- King Leopold's Ghost - Introduction
- PART ONE: DIS-EASE TREATMENT AND HEALTH-4
- PART ONE: DIS-EASE TREATMENT AND HEALTH-2
- PART ONE: DIS-EASE TREATMENT AND HEALTH-5
- African Wholistics - Medicine
- Menopause
- The Black Pharaohs Nubian Pharaohs of Ancient Egypt
- The Mystery System
- PART ONE: DIS-EASE TREATMENT AND HEALTH-6
Who's On Line?
We have 96 guests and no members online
Ad Agency Remote
Articles - Latest
- The Male G Spot Is Real—and It's the Secret to an Unbelievable Orgasm
- Herbs for Parasitic Infections
- Vaginal Care - From Pubes to Lubes: 8 Ways to Keep Your Vagina Happy
- 5 Negative Side Effects Of Anal Sex
- Your Herbs and Spices Might Contain Arsenic, Cadmium, and Lead
- Struggling COVID-19 Vaccines From AstraZeneca, BioNTech/Pfizer, Moderna Cut Incidence Of Arterial Thromboses That Cause Heart Attacks, Strokes, British Study Shows
- Cartilage comfort - Natural Solutions
- Stop Overthinking Now: 18 Ways to Control Your Mind Again
- Groundbreaking method profiles gene activity in the living brain
- Top 5 health benefits of quinoa
- Chromolaena odorata - Jackanna Bush
- Quickly Drain You Lymph System Using Theses Simple Techniques to Boost Immunity and Remove Toxins
- Doctors from Nigeria 'facing exploitation' in UK
- Amaranth, callaloo, bayam, chauli
- 9 Impressive Benefits of Horsetail
- Collagen The Age-Defying Secret Of The Stars + Popular Products in 2025
- Sarcopenia With Aging
- How to Travel as a Senior (20 Simple Tips)
- Everything you need to know about mangosteen













